Drug Catalog - Product Detail
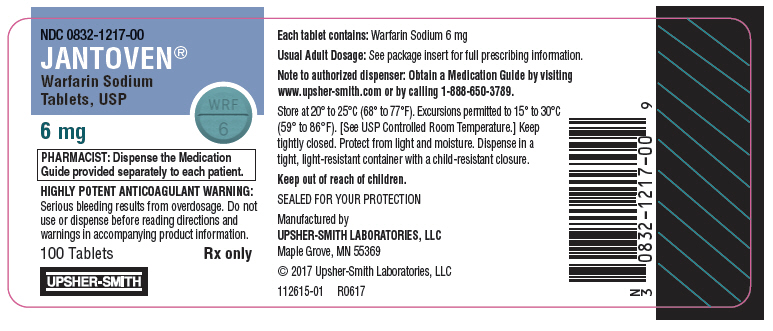
WARFARIN SODIUM, USP (JANTOVEN) TB 6MG 10X10 UD
| NDC | Mfr | Size | Str | Form |
|---|---|---|---|---|
| 00832-1217-01 | UPSHER-SMITH | 100 | 6MG | TABLET |
PACKAGE FILES
Generic Name
WARFARIN SODIUM
Substance Name
WARFARIN SODIUM
Product Type
HUMAN PRESCRIPTION DRUG
Route
ORAL
Application Number
ANDA040416
Description
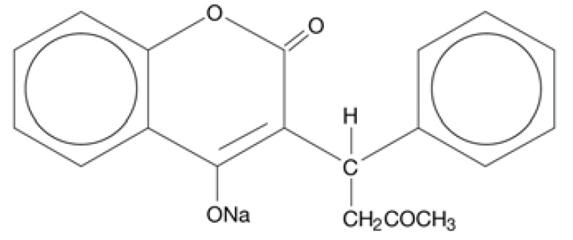
11 DESCRIPTION JANTOVEN (Warfarin Sodium Tablets, USP) is an anticoagulant that acts by inhibiting vitamin K-dependent coagulation factors. The chemical name of warfarin sodium is 3-(α-acetonylbenzyl)-4-hydroxycoumarin sodium salt, which is a racemic mixture of the R - and S -enantiomers. Crystalline warfarin sodium is an isopropanol clathrate. Its empirical formula is C 19 H 15 NaO 4 , and its structural formula is represented by the following: Crystalline warfarin sodium occurs as a white, odorless, crystalline powder that is discolored by light. It is very soluble in water, freely soluble in alcohol, and very slightly soluble in chloroform and ether. JANTOVEN tablets for oral use contain: 1 mg, 2 mg, 2½ mg, 3 mg, 4 mg, 5 mg, 6 mg, 7½ mg or 10 mg of warfarin sodium, USP. They also contain: All strengths: Lactose monohydrate, magnesium stearate, povidone, and pregelatinized starch (corn). 1 mg: FD&C Red #40 Aluminum Lake 2 mg: FD&C Blue #2 Aluminum Lake and FD&C Red #40 Aluminum Lake 2½ mg: D&C Yellow #10 Aluminum Lake and FD&C Blue #1 Aluminum Lake 3 mg: Brown #75 Synthetic Brown Iron Oxide 4 mg: FD&C Blue #1 Aluminum Lake 5 mg: FD&C Yellow #6 Aluminum Lake 6 mg: Yellow #10 Synthetic Yellow Iron Oxide, Black #85 Synthetic Black Iron Oxide and FD&C Blue #1 Aluminum Lake 7½ mg: D&C Yellow #10 Aluminum Lake and FD&C Yellow #6 Aluminum Lake 10 mg: Dye Free Chemical Structure
How Supplied
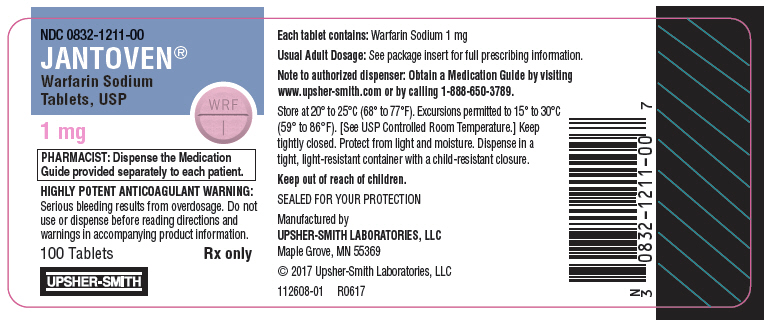
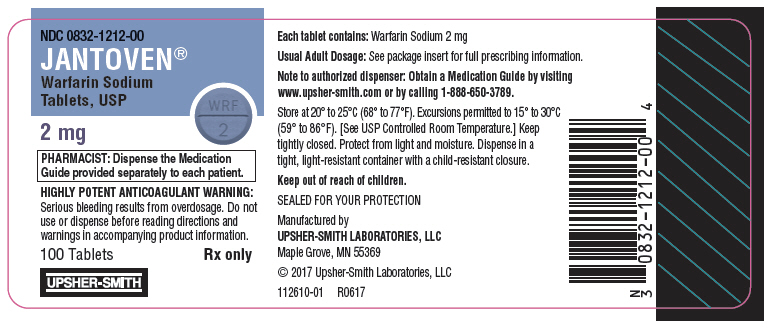
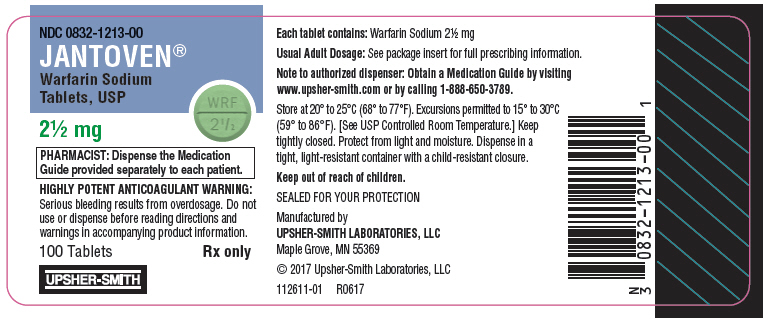
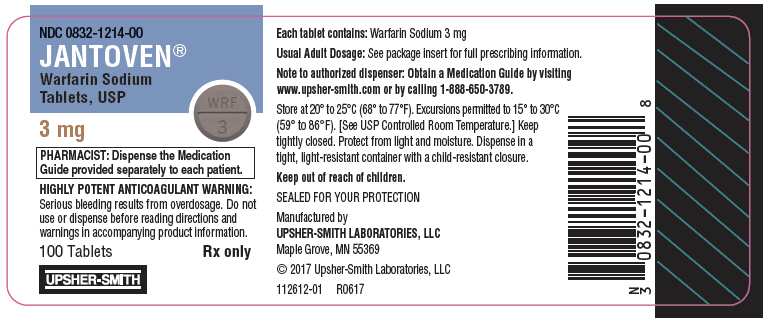
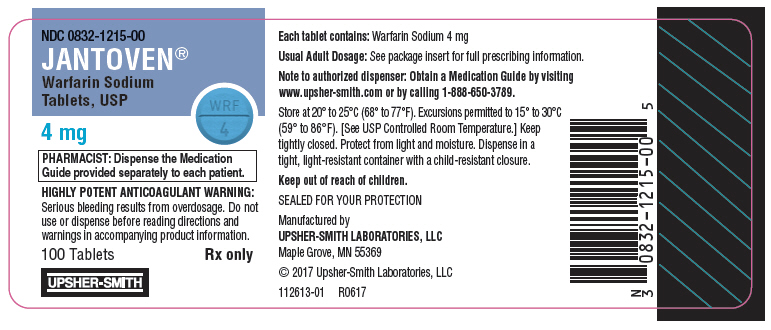
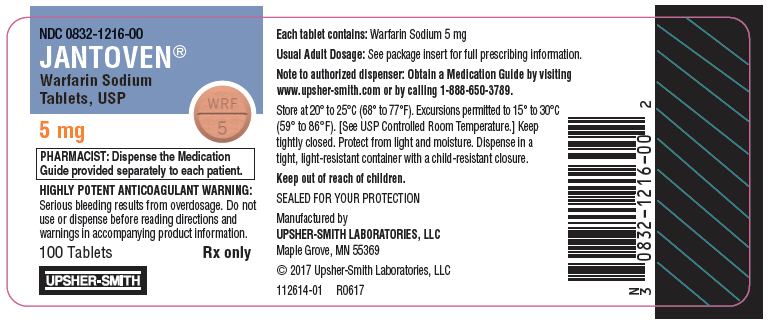
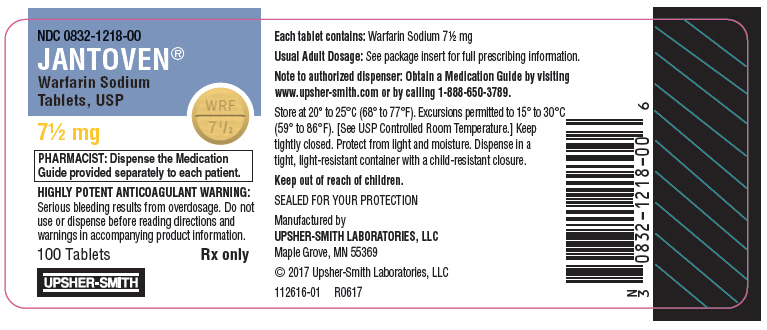
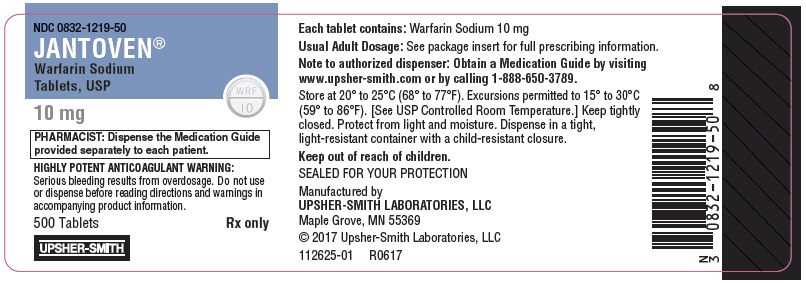
16 HOW SUPPLIED/STORAGE AND HANDLING Tablets JANTOVEN tablets are single scored, compressed tablets with one side scored and debossed with WRF above the score and 1, 2, 2½, 3, 4, 5, 6, 7½, or 10 below the score and with 832 debossed on the opposite side. JANTOVEN is available in bottles and unit dose blister packages with potencies and colors as follows: 1 mg – Compressed tablet, pink, round; in bottles of 100 (NDC 0832-1211-00) and 1000 (NDC 0832-1211-10) and in unit dose cartons of 100 tablets (10 cards containing 10 tablets each) (NDC 0832-1211-01). 2 mg – Compressed tablet, lavender, round; in bottles of 100 (NDC 0832-1212-00) and 1000 (NDC 0832-1212-10) and in unit dose cartons of 100 tablets (10 cards containing 10 tablets each) (NDC 0832-1212-01). 2½ mg – Compressed tablet, green, round; in bottles of 100 (NDC 0832-1213-00) and 1000 (NDC 0832-1213-10) and in unit dose cartons of 100 tablets (10 cards containing 10 tablets each) (NDC 0832-1213-01). 3 mg – Compressed tablet, tan, round; in bottles of 100 (NDC 0832-1214-00) and 1000 (NDC 0832-1214-10) and in unit dose cartons of 100 tablets (10 cards containing 10 tablets each) (NDC 0832-1214-01). 4 mg – Compressed tablet, blue, round; in bottles of 100 (NDC 0832-1215-00) and 1000 (NDC 0832-1215-10) and in unit dose cartons of 100 tablets (10 cards containing 10 tablets each) (NDC 0832-1215-01). 5 mg – Compressed tablet, peach, round; in bottles of 100 (NDC 0832-1216-00) and 1000 (NDC 0832-1216-10) and in unit dose cartons of 100 tablets (10 cards containing 10 tablets each) (NDC 0832-1216-01). 6 mg – Compressed tablet, teal, round; in bottles of 100 (NDC 0832-1217-00) and 1000 (NDC 0832-1217-10) and in unit dose cartons of 100 tablets (10 cards containing 10 tablets each) (NDC 0832-1217-01). 7½ mg – Compressed tablet, yellow, round; in bottles of 100 (NDC 0832-1218-00) and 500 (NDC 0832-1218-50) and in unit dose cartons of 100 tablets (10 cards containing 10 tablets each) (NDC 0832-1218-01). 10 mg – Compressed tablet, white (dye-free), round; in bottles of 100 (NDC 0832-1219-00) and 500 (NDC 0832-1219-50) and in unit dose cartons of 100 tablets (10 cards containing 10 tablets each) (NDC 0832-1219-01). Store at 20° to 25°C (68° to 77°F). Excursions permitted to 15° to 30°C (59° to 86°F). [See USP Controlled Room Temperature.] Protect from light and moisture. Dispense in a tight, light-resistant container with a child-resistant closure. Special Handling Procedures for proper handling and disposal of potentially hazardous drugs should be considered. Guidelines on this subject have been published [see References (15) ]. Pharmacy and clinical personnel who are pregnant should avoid exposure to crushed or broken tablets [see Use in Specific Populations (8.1) ].
Indications & Usage
1 INDICATIONS AND USAGE JANTOVEN ® is indicated for: Prophylaxis and treatment of venous thrombosis and its extension, pulmonary embolism (PE). Prophylaxis and treatment of thromboembolic complications associated with atrial fibrillation (AF) and/or cardiac valve replacement. Reduction in the risk of death, recurrent myocardial infarction (MI), and thromboembolic events such as stroke or systemic embolization after myocardial infarction. Limitations of Use Warfarin Sodium has no direct effect on an established thrombus, nor does it reverse ischemic tissue damage. Once a thrombus has occurred, however, the goals of anticoagulant treatment are to prevent further extension of the formed clot and to prevent secondary thromboembolic complications that may result in serious and possibly fatal sequelae. JANTOVEN is a vitamin K antagonist indicated for: Prophylaxis and treatment of venous thrombosis and its extension, pulmonary embolism ( 1 ) Prophylaxis and treatment of thromboembolic complications associated with atrial fibrillation and/or cardiac valve replacement ( 1 ) Reduction in the risk of death, recurrent myocardial infarction, and thromboembolic events such as stroke or systemic embolization after myocardial infarction ( 1 ) Limitations of Use Warfarin Sodium has no direct effect on an established thrombus, nor does it reverse ischemic tissue damage. ( 1 )
Dosage and Administration
2 DOSAGE AND ADMINISTRATION Individualize dosing regimen for each patient, and adjust based on INR response. ( 2.1 , 2.2 ) Knowledge of genotype can inform initial dose selection. ( 2.3 ) Monitoring: Obtain daily INR determinations upon initiation until stable in the therapeutic range. Obtain subsequent INR determinations every 1 to 4 weeks. ( 2.4 ) Review conversion instructions from other anticoagulants. ( 2.8 ) 2.1 Individualized Dosing The dosage and administration of JANTOVEN must be individualized for each patient according to the patient's International Normalized Ratio (INR) response to the drug. Adjust the dose based on the patient's INR and the condition being treated. Consult the latest evidence-based clinical practice guidelines regarding the duration and intensity of anticoagulation for the indicated conditions. 2.2 Recommended Target INR Ranges and Durations for Individual Indications An INR of greater than 4.0 appears to provide no additional therapeutic benefit in most patients and is associated with a higher risk of bleeding. Venous Thromboembolism (including deep venous thrombosis [DVT] and PE) Adjust the warfarin dose to maintain a target INR of 2.5 (INR range, 2.0 to 3.0) for all treatment durations. The duration of treatment is based on the indication as follows: For patients with a DVT or PE secondary to a transient (reversible) risk factor, treatment with warfarin for 3 months is recommended. For patients with an unprovoked DVT or PE, treatment with warfarin is recommended for at least 3 months. After 3 months of therapy, evaluate the risk-benefit ratio of long-term treatment for the individual patient. For patients with two episodes of unprovoked DVT or PE, long-term treatment with warfarin is recommended. For a patient receiving long-term anticoagulant treatment, periodically reassess the risk-benefit ratio of continuing such treatment in the individual patient. Atrial Fibrillation In patients with non-valvular AF, anticoagulate with warfarin to target INR of 2.5 (range, 2.0 to 3.0). In patients with non-valvular AF that is persistent or paroxysmal and at high risk of stroke (i.e., having any of the following features: prior ischemic stroke, transient ischemic attack, or systemic embolism, or 2 of the following risk factors: age greater than 75 years, moderately or severely impaired left ventricular systolic function and/or heart failure, history of hypertension, or diabetes mellitus), long-term anticoagulation with warfarin is recommended. In patients with non-valvular AF that is persistent or paroxysmal and at an intermediate risk of ischemic stroke (i.e., having 1 of the following risk factors: age greater than 75 years, moderately or severely impaired left ventricular systolic function and/or heart failure, history of hypertension, or diabetes mellitus), long-term anticoagulation with warfarin is recommended. For patients with AF and mitral stenosis, long-term anticoagulation with warfarin is recommended. For patients with AF and prosthetic heart valves, long-term anticoagulation with warfarin is recommended; the target INR may be increased and aspirin added depending on valve type and position, and on patient factors. Mechanical and Bioprosthetic Heart Valves For patients with a bileaflet mechanical valve or a Medtronic Hall (Minneapolis, MN) tilting disk valve in the aortic position who are in sinus rhythm and without left atrial enlargement, therapy with warfarin to a target INR of 2.5 (range, 2.0 to 3.0) is recommended. For patients with tilting disk valves and bileaflet mechanical valves in the mitral position, therapy with warfarin to a target INR of 3.0 (range, 2.5 to 3.5) is recommended. For patients with caged ball or caged disk valves, therapy with warfarin to a target INR of 3.0 (range, 2.5 to 3.5) is recommended. For patients with a bioprosthetic valve in the mitral position, therapy with warfarin to a target INR of 2.5 (range, 2.0 to 3.0) for the first 3 months after valve insertion is recommended. If additional risk factors for thromboembolism are present (AF, previous thromboembolism, left ventricular dysfunction), a target INR of 2.5 (range, 2.0 to 3.0) is recommended. Post-Myocardial Infarction For high-risk patients with MI (e.g., those with a large anterior MI, those with significant heart failure, those with intracardiac thrombus visible on transthoracic echocardiography, those with AF, and those with a history of a thromboembolic event), therapy with combined moderate-intensity (INR, 2.0 to 3.0) warfarin plus low-dose aspirin (≤100 mg/day) for at least 3 months after the MI is recommended. Recurrent Systemic Embolism and Other Indications Oral anticoagulation therapy with warfarin has not been fully evaluated by clinical trials in patients with valvular disease associated with AF, patients with mitral stenosis, and patients with recurrent systemic embolism of unknown etiology. However, a moderate dose regimen (INR 2.0 to 3.0) may be used for these patients. 2.3 Initial and Maintenance Dosing The appropriate initial dosing of JANTOVEN varies widely for different patients. Not all factors responsible for warfarin dose variability are known, and the initial dose is influenced by: Clinical factors including age, race, body weight, sex, concomitant medications, and comorbidities Genetic factors (CYP2C9 and VKORC1 genotypes) [see Clinical Pharmacology (12.5) ] Select the initial dose based on the expected maintenance dose, taking into account the above factors. Modify this dose based on consideration of patient-specific clinical factors. Consider lower initial and maintenance doses for elderly and/or debilitated patients and in Asian patients [see Use in Specific Populations (8.5) and Clinical Pharmacology (12.3) ]. Routine use of loading doses is not recommended as this practice may increase hemorrhagic and other complications and does not offer more rapid protection against clot formation. Individualize the duration of therapy for each patient. In general, anticoagulant therapy should be continued until the danger of thrombosis and embolism has passed [see Dosage and Administration (2.2) ]. Dosing Recommendations without Consideration of Genotype If the patient's CYP2C9 and VKORC1 genotypes are not known, the initial dose of JANTOVEN is usually 2 to 5 mg once daily. Determine each patient's dosing needs by close monitoring of the INR response and consideration of the indication being treated. Typical maintenance doses are 2 to 10 mg once daily. Dosing Recommendations with Consideration of Genotype Table 1 displays three ranges of expected maintenance JANTOVEN doses observed in subgroups of patients having different combinations of CYP2C9 and VKORC1 gene variants [see Clinical Pharmacology (12.5) ]. If the patient's CYP2C9 and/or VKORC1 genotype are known, consider these ranges in choosing the initial dose. Patients with CYP2C9 *1/*3, *2/*2, *2/*3, and *3/*3 may require more prolonged time (>2 to 4 weeks) to achieve maximum INR effect for a given dosage regimen than patients without these CYP variants. Table 1: Three Ranges of Expected Maintenance JANTOVEN Daily Doses Based on CYP2C9 and VKORC1 Genotypes Ranges are derived from multiple published clinical studies. VKORC1–1639G>A (rs9923231) variant is used in this table. Other co-inherited VKORC1 variants may also be important determinants of warfarin dose. VKORC1 CYP2C9 *1/*1 *1/*2 *1/*3 *2/*2 *2/*3 *3/*3 GG 5–7 mg 5–7 mg 3–4 mg 3–4 mg 3–4 mg 0.5–2 mg AG 5–7 mg 3–4 mg 3–4 mg 3–4 mg 0.5–2 mg 0.5–2 mg AA 3–4 mg 3–4 mg 0.5–2 mg 0.5–2 mg 0.5–2 mg 0.5–2 mg 2.4 Monitoring to Achieve Optimal Anticoagulation JANTOVEN has a narrow therapeutic range (index), and its action may be affected by factors such as other drugs and dietary vitamin K. Therefore, anticoagulation must be carefully monitored during JANTOVEN therapy. Determine the INR daily after the administration of the initial dose until INR results stabilize in the therapeutic range. After stabilization, maintain dosing within the therapeutic range by performing periodic INRs. The frequency of performing INR should be based on the clinical situation but generally acceptable intervals for INR determinations are 1 to 4 weeks. Perform additional INR tests when other warfarin products are interchanged with JANTOVEN, as well as whenever other medications are initiated, discontinued, or taken irregularly. Heparin, a common concomitant drug, increases the INR [see Dosage and Administration (2.8) and Drug Interactions (7) ]. Determinations of whole blood clotting and bleeding times are not effective measures for monitoring of JANTOVEN therapy. 2.5 Renal Impairment No dosage adjustment is necessary for patients with renal failure. Monitor INR more frequently in patients with compromised renal function to maintain INR within the therapeutic range [see Warnings and Precautions (5.4) and Use in Specific Populations (8.6) ]. 2.6 Missed Dose The anticoagulant effect of JANTOVEN persists beyond 24 hours. If a patient misses a dose of JANTOVEN at the intended time of day, the patient should take the dose as soon as possible on the same day. The patient should not double the dose the next day to make up for a missed dose. 2.7 Treatment during Dentistry and Surgery Some dental or surgical procedures may necessitate the interruption or change in the dose of JANTOVEN therapy. Consider the benefits and risks when discontinuing JANTOVEN even for a short period of time. Determine the INR immediately prior to any dental or surgical procedure. In patients undergoing minimally invasive procedures who must be anticoagulated prior to, during, or immediately following these procedures, adjusting the dosage of JANTOVEN to maintain the INR at the low end of the therapeutic range may safely allow for continued anticoagulation. 2.8 Conversion from Other Anticoagulants Heparin Since the full anticoagulant effect of JANTOVEN is not achieved for several days, heparin is preferred for initial rapid anticoagulation. During initial therapy with JANTOVEN, the interference with heparin anticoagulation is of minimal clinical significance. Conversion to JANTOVEN may begin concomitantly with heparin therapy or may be delayed 3 to 6 days. To ensure therapeutic anticoagulation, continue full dose heparin therapy and overlap JANTOVEN therapy with heparin for 4 to 5 days and until JANTOVEN has produced the desired therapeutic response as determined by INR, at which point heparin may be discontinued. As heparin may affect the INR, patients receiving both heparin and JANTOVEN should have INR monitoring at least: 5 hours after the last intravenous bolus dose of heparin, or 4 hours after cessation of a continuous intravenous infusion of heparin, or 24 hours after the last subcutaneous heparin injection. JANTOVEN may increase the activated partial thromboplastin time (aPTT) test, even in the absence of heparin. A severe elevation (>50 seconds) in aPTT with an INR in the desired range has been identified as an indication of increased risk of postoperative hemorrhage. Other Anticoagulants Consult the labeling of other anticoagulants for instructions on conversion to JANTOVEN.
